Advocating for Yourself: My Epilepsy Journey
My name is Natalie, and I’ve been working with the Grand Rapids LGBTQ+ Healthcare Consortium since September 2024 as the Program Coordinator. Today is my last day with the Consortium — and since November is Epilepsy Awareness Month, I wanted to take this opportunity to share my own epilepsy journey.
When I was about 14 or 15, I started having seizures — though at the time, no one knew that’s what they were. It took nearly two years before I received a proper diagnosis.
Every single seizure was the same: I would put my hands around my throat and start making a choking noise. I never had the convulsions most people imagine when they hear the word “seizure.” Because of that, my episodes didn’t look like the “typical” kind you see in movies or on TV, which made it harder for my friends and my mom to understand what was happening — but it shouldn’t have been hard for a doctor to recognize.
One night, I was having a sleepover with a friend when she woke up because I was choking. She said I sat up, put my hands around my throat, and started making that same strange noise. She tried to wake me, but I wouldn’t respond. She ran to get my mom, and by the time they returned, the episode had stopped.
My mom took me to my pediatrician and explained what happened. Neither of us can remember exactly what was said at that appointment, but no treatment was recommended. Since it happened at night, the doctor referred us to a sleep clinic.
The sleep specialists asked my mom to try to capture one of the episodes on video. So she started sleeping next to me, and whenever I’d have an episode, she’d grab her phone and try to record it. Of course, it was the middle of the night and she was half asleep — so she was never able to get a clear video. She was convinced they were seizures, but the clinic wasn’t sure and ordered a sleep study.
During the sleep study, I had another episode. The sleep doctor, however, did not recognize it as a seizure. Instead, he diagnosed me with sleep apnea, despite my mom’s concerns. I was prescribed a CPAP machine, but because it was a misdiagnosis, the episodes didn’t stop.
At that time, I also wasn’t getting good sleep — because, as we later learned, I was having seizures almost every night. I was exhausted, confused, and frustrated, and no one could tell us why. It was an incredibly difficult time. The seizures kept happening night after night while my mom was repeatedly told it was just sleep apnea.
When I was 17, I started having seizures during the day. The same thing would happen, but now I was awake beforehand. The first daytime seizure happened at school. A group of kids helped me to the office, where the staff called my mom. (I have no memory of this — I was in class one minute, and the next, I was in the front office with my mom sitting next to me asking if I was okay.) She came to pick me up and took me straight to the pediatrician.
On the way, I had another seizure in the car. Then, once we got to the doctor’s office, I had yet another one — right in front of him. He immediately said, “That’s a seizure.” Finally, I was referred to a neurologist.
After an EEG and a hospital stay, I was officially diagnosed with focal epilepsy. I had been having left temporal lobe focal seizures every single night for nearly two years. The neurologists couldn’t believe the sleep doctor had thought it was sleep apnea — to them, it was clearly a seizure disorder.
They started me on medication, and since the day I was diagnosed, I haven’t had a seizure.
I’m 28 now and have been seizure-free for over 11 years. While I still experience a few side effects, epilepsy does not define my daily life.
If there’s one thing I’ve learned from my journey, it’s this: always advocate for yourself.
At the time, I couldn’t — I was under 18 and had no memory of my seizures. My mom did everything she could, even when she was told over and over that she was wrong. She knew something wasn’t right and never stopped pushing for answers.
Your doctor may be an expert, but you are the expert on your own body. Don’t be afraid to speak up, ask questions, or seek a second opinion. You deserve to be heard, believed, and cared for.
The Importance of Black People within the LGBTQ+ Community: A Tribute to Pioneers and Activists
In honor of Black History Month, this blog post celebrates the essential role Black individuals have played in shaping the LGBTQ+ community. Despite facing the dual challenges of racial and gender or sexual discrimination, Black people have been at the forefront of the fight for civil rights, social justice, and LGBTQ+ equality. Their impact, from the pioneering work of Black trans women to the contributions of Black LGBTQ+ activists, has been foundational in the progress we see today.
While the LGBTQ+ rights movement has always intersected with issues of race and identity, the contributions of Black people—especially Black trans women—are often overlooked in mainstream history. These trailblazers have not only shaped LGBTQ+ advocacy but have provided vital leadership and resilience that continue to influence the movement. This post highlights the rich history of Black LGBTQ+ figures whose activism and leadership have left an indelible mark on the community.
Historical Context: Intersectionality in the LGBTQ+ Movement
The fight for LGBTQ+ rights has always been deeply intertwined with the struggle for racial justice. Black LGBTQ+ individuals have faced a unique set of challenges due to their race and sexual or gender identities. For many years, this intersectionality has meant being excluded from both mainstream LGBTQ+ spaces and traditional civil rights movements. Yet, it is these very individuals who have helped define and strengthen the movement we see today. The contributions of Black LGBTQ+ people, especially those at the intersections of race, gender, and sexuality, have been crucial to advancing both civil and human rights.
Pioneers in the LGBTQ+ Rights Movement: The Foundational Figures
One of the most pivotal moments in LGBTQ+ history was the 1969 Stonewall Riots. While Marsha P. Johnson and Sylvia Rivera are often celebrated as foundational figures in this movement, it is essential to recognize the broader scope of Black LGBTQ+ contributions to the fight for equality.
Marsha P. Johnson: A Revolutionary Figure
Marsha P. Johnson, a Black trans woman and drag queen, was one of the most important figures in the Stonewall Riots. Along with Sylvia Rivera, she co-founded the Street Transvestite Action Revolutionaries (STAR), an organization dedicated to advocating for homeless queer and trans people. Marsha’s leadership, particularly in pushing for the inclusion of marginalized groups within the LGBTQ+ movement, helped to lay the foundation for modern-day trans activism.
Her advocacy didn’t just influence the rights of transgender individuals—it reshaped the way we think about intersectional activism, where race, gender, and sexual identity are all part of the fight for justice and equality.
Sylvia Rivera: A Fierce Ally and Advocate
Sylvia Rivera, an LGBTQ+ rights activist, also played a crucial role in the early LGBTQ+ rights movement. Alongside Marsha, she worked tirelessly to create spaces for marginalized communities, particularly trans and queer people of color, who had long been excluded from the larger LGBTQ+ movement. Despite facing significant opposition from within the movement itself, Sylvia’s commitment to trans and queer inclusion made her a key figure in ensuring the voices of the most marginalized were heard.
Rivera’s legacy as an advocate for trans rights and inclusivity continues to inspire those who fight for visibility and equality today.
Additional Pioneers Who Shaped the Movement
Beyond Johnson and Rivera, many other Black LGBTQ+ figures have made significant contributions to the struggle for rights and recognition. These activists laid the groundwork for the fight for LGBTQ+ liberation we continue to carry on today.
Bayard Rustin: A Civil Rights and LGBTQ+ Leader
Bayard Rustin (1912–1987), a civil rights strategist and one of the principal organizers of the 1963 March on Washington for Jobs and Freedom, was instrumental in shaping the civil rights movement. Though Rustin was openly gay, his sexuality was often overlooked or downplayed within mainstream civil rights spaces. Nevertheless, he made a lasting impact by advocating for both racial and LGBTQ+ equality, proving that these struggles are deeply interconnected. In 2019, the movie Rustin was released, focusing on his life and legacy, highlighting his pivotal role in the movement and his resilience in the face of discrimination. The film brought renewed attention to Rustin’s contributions and the intersectionality of his activism, celebrating his courage and the complexity of his identity as a Black gay man who helped shape one of the most significant moments in American history.
Frances Thompson: A Trailblazer for Black LGBTQ+ Rights
Frances Thompson (1857-1925) was a pioneering Black trans activist, is thought to be the first trans woman to testify before Congress, advocating for the rights and dignity of transgender individuals. Born into slavery in the 1850s, Thompson’s life spanned eras of immense social change, and her courage in publicly embracing her identity during times of racial and gender discrimination made her a crucial figure in both the Black and LGBTQ+ rights movements. Her testimony before Congress helped highlight the unique challenges faced by Black transgender individuals, ensuring intersectionality was central to the fight for justice. Though often overlooked, Thompson's legacy continues to inspire those working toward equality today.
Audre Lorde: Poet, Feminist, and Revolutionary
Audre Lorde (1934–1992) was a Black lesbian poet and activist whose work focused on the intersections of race, gender, and sexuality. Lorde’s poetry, essays, and activism challenged societal norms and called for radical self-love and inclusion. Through her writing, she emphasized the importance of addressing both the visible and invisible aspects of identity—how race, gender, and sexuality all converge to shape our experiences.
Her work continues to influence both feminist and LGBTQ+ movements, providing a blueprint for those who seek to build an inclusive world for all people.
James Baldwin: A Literary Giant
James Baldwin (1924–1987) was a novelist, essayist, and playwright whose work explored the complexities of race, sexuality, and identity in America. Baldwin’s personal exploration of his queer identity and his profound insights into the Black experience in America made him a pivotal figure in both the LGBTQ+ and civil rights movements.
Baldwin’s eloquent writing challenged societal norms and sparked important conversations about the intersections of race, gender, and sexuality. His influence endures, and his work continues to inspire activists and writers today.
Black LGBTQ+ Activism Today: Continuing the Fight
The LGBTQ+ movement continues to be shaped by the work of Black activists who carry forward the legacies of those who came before them. Figures such as Brittney Griner, Raquel Willis, Laverne Cox, and Billy Porter are among those raising awareness on crucial issues like police brutality, access to healthcare, and the rights of LGBTQ+ youth.
Laverne Cox: A Groundbreaking Advocate for Black Trans Visibility
Laverne Cox, a groundbreaking actress and advocate, has used her platform to amplify the visibility of Black trans women and challenge harmful stereotypes about transgender people. As the first openly transgender woman of color nominated for a Primetime Emmy Award, Cox has been instrumental in reshaping how trans individuals—particularly trans people of color—are portrayed in mainstream media. Her advocacy extends beyond acting, as she continues to be a fierce voice for trans rights and inclusion in all aspects of society.
Brittney Griner: A Symbol of Resilience and Advocacy
Brittney Griner, the WNBA star who became a symbol of resilience after her wrongful detention in Russia, has also been an advocate for both racial justice and LGBTQ+ rights. Griner's public journey has highlighted the intersections of race, gender, and sexuality, emphasizing the need for solidarity across movements. As a Black queer woman, Griner’s courage has empowered others to speak out about issues related to justice, equality, and the rights of LGBTQ+ people.
Raquel Willis: Amplifying Black Trans Voices
Raquel Willis, a Black trans activist and writer, has been a fierce advocate for the rights and visibility of Black trans individuals. Through her work, she has shed light on the unique challenges faced by Black trans people, particularly around issues of safety, healthcare, and justice. Willis’s advocacy emphasizes the importance of centering the voices of Black trans people in broader conversations about LGBTQ+ rights and inclusion.
Billy Porter: Breaking Barriers in Fashion and Entertainment
Billy Porter, a renowned actor and fashion icon, has shattered expectations with his bold approach to gender expression. Through his roles, activism, and public appearances, Porter has become an advocate for Black queer people, championing their representation and inclusion in the entertainment industry and beyond. His fearless exploration of fashion and gender norms has made him a powerful figure in reshaping how the world views Black LGBTQ+ individuals.
Conclusion: Honoring the Legacy of Black LGBTQ+ Pioneers
The contributions of Black LGBTQ+ individuals—both past and present—have been instrumental in shaping the ongoing fight for equality. From the groundbreaking work of Marsha P. Johnson and Sylvia Rivera to the literary brilliance of James Baldwin and Audre Lorde, these pioneers have paved the way for generations of LGBTQ+ activists. Today, figures like Billy Porter, and Brittney Griner continue to push boundaries and advocate for justice, visibility, and inclusion. Their commitment to justice and the ongoing fight for LGBTQ+ liberation continues to inspire movements today, reminding us that the struggle for liberation is a collective one.
As we continue to move forward, it’s essential to honor and uplift the voices of Black LGBTQ+ individuals, ensuring that their legacies are preserved and their contributions are never forgotten. Their activism and courage have shaped the LGBTQ+ movement into what it is today, and their work is far from finished.
Let’s celebrate and continue to amplify the voices of Black LGBTQ+ leaders who continue to fight for a more inclusive, just, and equal world for all.
Resources
Street Transvestite Action Revolutionaries(STAR) Manifesto
Audre Lorde Books and Writings
navigating the holidays as an lgbtq+ person
While the holiday season can be a time of celebration and joy, it’s also a period that can bring heightened emotions, stress, and discomfort, especially for members of the LGBTQ+ community. Although research shows no significant spike in mental health struggles during the holidays, existing conditions may be exacerbated, particularly for individuals without supportive family or a safe network.
A 2014 survey by the National Alliance on Mental Illness revealed that 64% of people with mental health challenges report that the holiday season makes their conditions worse. For 24% of people, the "holiday blues" make things significantly harder. These heightened emotional experiences are even more relevant for LGBTQ+ individuals, who face a higher risk of mental health conditions compared to heterosexual people. According to the National Survey on Drug Use and Health, lesbian, gay, and bisexual adults are more than twice as likely to experience mental health struggles, while transgender people are nearly four times as likely to face such challenges.
So, let’s talk about the struggles this community faces and some tips for those who may need extra support.
5 Common Holiday Challenges for LGBTQ+ Individuals
Lack of Acceptance: Some LGBTQ+ individuals may still be in the process of coming out or have faced rejection in the past. Returning home can stir up painful memories, triggering feelings of shame and guilt.
Microaggressions: Family members, even if well-intentioned, may make subtle or unintentional comments that are offensive or dismissive of LGBTQ+ identities. These microaggressions can be hurtful and add to the discomfort of an unsupportive family environment.
Misgendering/Deadnaming: For transgender and non-binary individuals, the holidays may bring repeated misgendering or deadnaming from family members who don't understand or respect their gender identity or chosen name. This can feel deeply invalidating and damaging.
Isolation: Not all LGBTQ+ individuals have supportive or accepting social networks. For those estranged from their families or with limited community connections, the holidays can highlight feelings of loneliness.
Mental Health Struggles: Feelings of anxiety, depression, and isolation can become more intense during the holiday season, particularly for those already dealing with stigma or discrimination.
5 Strategies for Nurturing Mental Health and Creating Safe Spaces
Although the holiday season can be challenging, there are ways to protect your mental health and create a sense of safety. Here are some tips to help:
Reflect on Your Needs and Set Boundaries: Before heading home, take time to reflect on what you want from the holiday season and what you need to avoid. Setting boundaries is essential. It’s important to communicate your needs for respect and understanding, especially when sensitive topics arise. You have the right to feel safe and accepted.
Build a Supportive Community: If your family isn't supportive, it's vital to connect with others who affirm your identity. Consider organizing get-togethers with trusted friends, or chosen family.
Create Safe Spaces at Home: For those who didn’t grow up in supportive households, creating your own sanctuary at home is vital for mental health and healing. Remember: your home should be a place where you can rest, recharge and feel valued.
Practice Self-Care: Make time for activities that nurture your mental health. Self-care can help you stay grounded during stressful times. Treat yourself! You deserve it!
Take Breaks and Manage Stress: It’s okay to step away from situations that feel overwhelming. Simple techniques like deep breathing, taking short walks, or visualizing a peaceful place can help reduce anxiety and stress.
Moving Forward
It’s important to acknowledge that many LGBTQ+ people face systemic challenges throughout the year, but the holiday season often magnifies these struggles. For those who might not feel safe or affirmed in their families, the holiday season can be a reminder of what is lacking, but also of what can be built. We can create our own families of choice, our own affirming spaces, and our own traditions of love and support. If you’re struggling, please know that you’re not alone, and resources like The Trevor Project are always available to provide support and guidance.
The holiday season should be a time of joy, and although it may not always feel that way, we can create the space for peace, love, and authenticity — for ourselves and for those who share our journey.
If you are struggling this season don’t hesitate to reach out for help! There are so many people who want what’s best for you and who are there for you 24/7. Check out the resources linked below.
Resources
The Trevor Project: (866) 488-7386
The LGBT National Hotline: (888) 843-4564, 1 on 1 Peer Support Chat
The Transgender Crisis Hotline: (877) 565-8860
National Suicide Prevention Lifeline: 988
Understanding Trans Lives: A Deep Dive for Transgender Awareness Week
Transgender Awareness Week is an important time for reflection, recognition, and advocacy within the transgender community and among allies. This week is not only about celebrating the accomplishments of transgender individuals but also to amplify their voices and highlight the unique challenges they face.
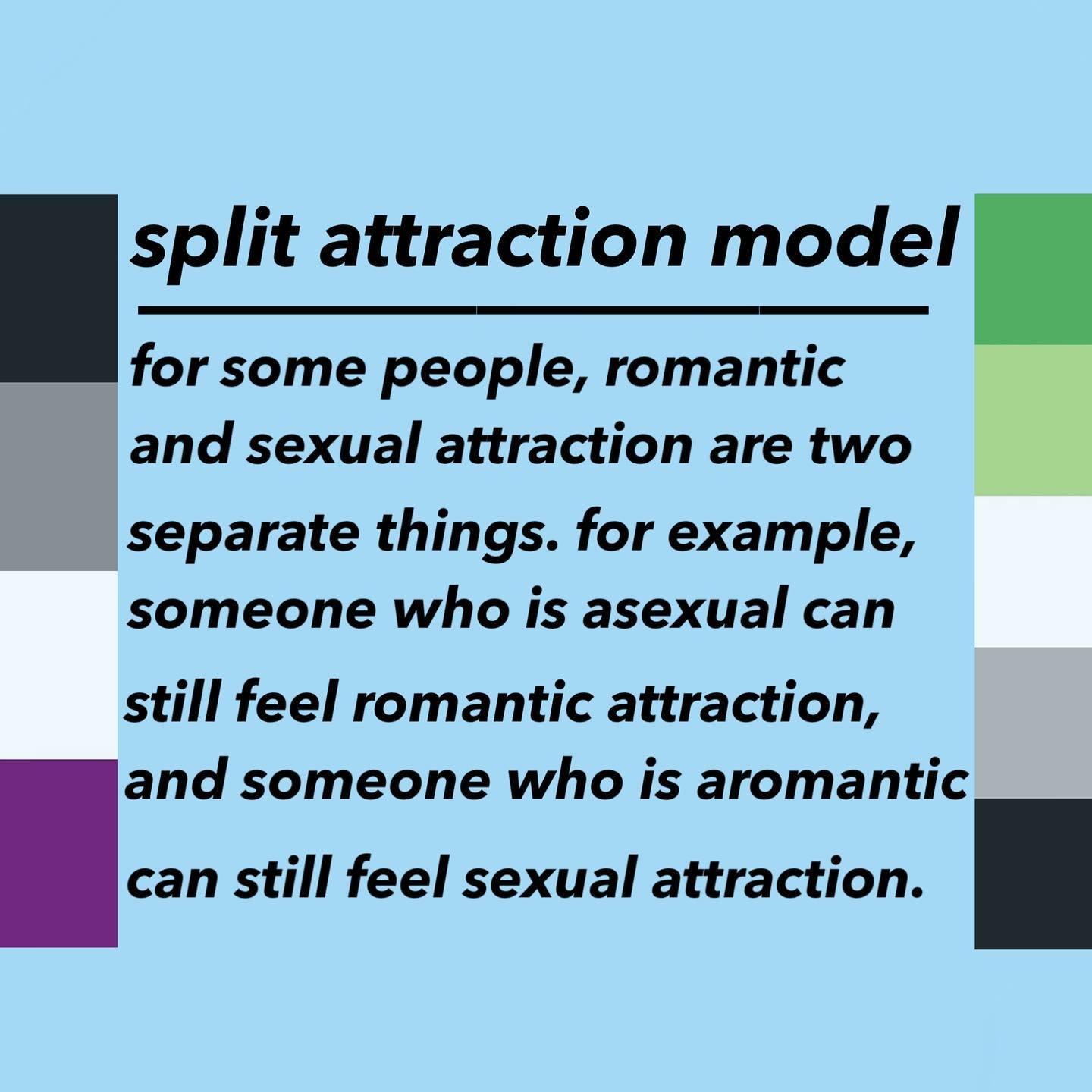
Understanding Transgender Identity
Being transgender refers to individuals whose gender identity differs from the sex they were assigned at birth. This identity exists independently of biological sex and often comes with a desire to transition to the gender that aligns with their true selves, the gender they identify with. Transgender people may identify as female, male, nonbinary, gender non-conforming, or embrace other gender identities that differ from the traditional binary framework. It’s essential to recognize that being transgender is about authenticity and self-recognition, reflecting a diverse spectrum of experiences and expressions within the entire human experience. Understanding and respecting these identities is important when it comes to fostering acceptance, affirmation, and inclusivity in our communities.
The Origins of Transgender Awareness Week
Transgender Awareness Week is an annual event that began in 2017 with the aim of highlighting the challenges faced by transgender individuals. Established to celebrate the achievements, talents, and contributions of transgender people globally, the week serves as a platform for advocacy and education. It takes place in November, strategically coinciding with Transgender Day of Remembrance, which honors the lives lost to transphobia and violence. This alignment underscores the dual purpose of the week: to recognize the resilience of the transgender community while also acknowledging the urgent need for social change and justice. Through awareness and activism, Transgender Awareness Week continues to foster greater understanding of gender diversity.
Recognizing Accomplishments
Throughout history, transgender individuals have made significant contributions to society in various fields, including art, science, politics, and activism. Transgender Awareness Week provides an opportunity to shine a light on these achievements, honoring those who have paved the way for greater acceptance and understanding. By sharing stories of success, we inspire others and demonstrate the resilience and strength of the transgender community.
Promoting Visibility
Visibility is a powerful tool in combating prejudice and discrimination. Transgender Awareness Week encourages everyone—transgender individuals and allies alike—to engage in conversations about gender identity and expression. Increased visibility helps normalize transgender experiences and fosters a sense of belonging. When people see diverse representations of gender in media, workplaces, and communities, it helps to challenge stereotypes and misconceptions.
Educating on Rights Issues
Education is at the heart of Transgender Awareness Week. Many people still lack a clear understanding of transgender rights and the specific issues faced by this community. From healthcare access and legal recognition to workplace discrimination and violence, the challenges are significant. By providing information and resources, we can empower individuals to advocate for change and support transgender rights.
Taking Action
As we observe Transgender Awareness Week, let us commit to being allies in this journey. Whether it’s attending events, engaging in educational activities, or simply listening to and uplifting transgender voices, every action counts. We can work to create a more inclusive world where everyone, regardless of their gender identity, can thrive.
What is Transgender Day of Remembrance?
Transgender Day of Remembrance (TDOR) is a poignant observance established in 1999 by transgender advocate Gwendolyn Ann Smith. It began as a vigil to honor Rita Hester, a transgender woman tragically murdered in 1998. This vigil aimed to commemorate not only Rita but also all transgender individuals who have lost their lives to violence, highlighting the systemic issues and prejudice faced by the transgender community. Over the years, TDOR has evolved into a powerful annual event that fosters remembrance, awareness, and advocacy, bringing people together to honor the lives taken and to reinforce the need for continued action against anti-transgender violence and discrimination. Each year, communities across the globe gather to reflect, mourn, and commit to creating a safer, more inclusive world for all.
“Transgender Day of Remembrance seeks to highlight the losses we face due to anti-transgender bigotry and violence. I am no stranger to the need to fight for our rights, and the right to simply exist is first and foremost. With so many seeking to erase transgender people — sometimes in the most brutal ways possible — it is vitally important that those we lose are remembered, and that we continue to fight for justice.”
– Gwendolyn Ann Smith (Transgender Day of Remembrance founder)
Transgender Day of Remembrance 2024
Listed below are the names of the 28 transgender individuals (that we know of) who have been tragically killed in the US in 2024 (as of 10/25/24). Click on each name to learn more about each of their lives and the circumstances of their deaths. We must continue to say their names and share their stories to ensure they are never forgotten. We must also advocate for change to help prevent these acts of violence from happening in the future.
(Content Warning: These articles contain discussions of violence against and details surrounding the deaths of transgender individuals.)
Kitty Monroe(43)-Sasha Williams(36)-África Parrilla García(25)-Righteous Torrence “TK” Hill(35)-Reyna Hernandez(54)-Diamond Brigman(36)- Alex “Boo” Taylor Franco(21)-Meraxes Medina(24)-Yella Clark(45)-River Nevaeh Goddard(17)-Tee “Lagend Billions” Arnold(36)-Starr Brown-Andrea Doria Dos Passos(37)-Kita Bee(46)-Jazlynn Johnson(18)-Tayy Dior Thomas(17)- Michelle Henry(25)-Liara Kaylee Tsai(35)-Pauly Likens(14)-Kenji Spurgeon(23)-Shannon Boswell(30)-Monique Brooks(49)-Dylan Gurley(20)-Tai’Von Lathan(24)- Kassim Omar(29)-Redd(25)-Honee Daniels(37)-Nex Benedict(16)
Resources
How to be an Ally to Transgender and Nonbinary Youth
What does it mean to “come out”?
October 11th was National Coming Out Day! Let’s talk about what it means to come out and what it means when a loved one comes out to you. Coming out is a significant and often transformative process for those who identify as LGBTQ+. At its core, coming out refers to the journey of acknowledging and accepting one’s sexual orientation or gender identity and then sharing that identity with others. This act can range from a deeply personal revelation to a public declaration, and it’s important to understand that each individual’s experience is unique. You might have encountered discussions about “coming out” that seem overly simplistic, judgmental, or even intimidating. The reality is that there isn’t a single way to come out or live openly. There may be some individuals in our lives with whom we wish to share our sexual orientation or gender identity, while there are others with whom we might not feel safe or comfortable disclosing that information. And that’s completely fine!
A Personal Journey
Coming out is not just a single event; lots of folks find themselves coming out many times to many different people, whether it's sharing your identity with a close friend online, confiding in a family member, or telling a partner; it's a multifaceted journey that can evoke a wide array of emotions. Many people feel a mix of fear and anxiety, but also relief and elation as they embrace their true selves. The courage it takes to come out cannot be overstated; it often involves vulnerability and a deep introspection about one’s identity.
The Process of Coming Out
For most, the first step in coming out is acknowledging one’s identity to oneself. This self-acceptance is crucial, as it lays the foundation for sharing that identity with others. After this internal recognition, the next steps often involve sharing with close friends, family, and community members. The timing and method of coming out vary greatly; some may choose to do so quickly, while others take their time.
Navigating Risks and Rewards
Deciding to come out is a highly personal choice that must consider various factors. While coming out can foster deeper connections and a sense of freedom, it also carries risks. Individuals may face potential backlash, emotional upheaval, or even physical danger, depending on their environment and the people in their lives.
Before coming out, it’s vital to weigh the potential consequences. Questions to consider include: Will coming out jeopardize your emotional or financial support from loved ones? Is there a risk of physical harm? Are you facing pressure to conform to expectations? If the answers to these questions lean toward concern, it may be wise to wait or seek additional support before taking this step.
Empowering Your Experience
Ultimately, the decision to come out is yours alone. You have the power to choose how, when, and with whom to share your identity. Many find it helpful to start this journey within supportive communities, whether that be through LGBTQ+ groups, online forums, or trusted friends. Surrounding yourself with understanding individuals can provide the comfort and encouragement needed to navigate this path.
Coming out is a personal journey that can bring immense growth and connection, but it’s also one that should be approached with care and consideration. Remember, you are in charge of your narrative, and your journey is valid—no matter how it unfolds.
What to say/do when someone comes out to you
Your response should depend on your relationship with the person, but there are some universally supportive actions you can take.
Thank Them- Express your appreciation for their trust by saying something like, “Thank you for sharing this with me.” It is a meaningful gift when someone feels confident enough to confide in you. You can also check in on how they feel about sharing this part of their identity.
Ask About Pronouns- If someone comes out as transgender, nonbinary, or gender-diverse, ask which pronouns they use. Use “use” rather than “prefer,” as the latter implies that correct pronoun usage is optional rather than essential. Pro-tip: It’s helpful to ask people about their pronouns in everyday situations, not just after they come out. Sharing your own pronouns can also create an inclusive environment.
Show Support- Inquire about how they would like to be supported, as some may want ongoing support while others prefer to move on. Remember not to act surprised, as this can imply that you didn’t consider their queerness or trans identity as a possibility. It’s also okay to ask about their coming out journey and what it has been like for them, but don’t get offended if they do not want to elaborate.
Offer Them a Way Out- If you want to ask about their identity, ensure they know they aren’t obligated to answer. Phrases like, “Is it okay if I ask you about this?” can help. Providing context for your questions can also be beneficial—for instance, explaining your interest based on a similar experience, while remembering not to make it about you.
Use Ring Theory- If you’re grappling with emotions about someone’s coming out, it’s important not to place that burden on them.
What NOT to say/do when someone comes out to you
Avoid Outing- When someone confides in you about their LGBTQ+ identity, never share that information with others without their explicit permission. Respect their right to control their own narrative, as outing someone can have serious repercussions in their personal and professional lives. Instead, aim to be a confidential and safe person for them, recognizing that coming out is a deeply personal choice and that being entrusted with this information is a privilege.
Respect Privacy- Don’t pry into details that haven’t been voluntarily shared. Maintain a respectful distance regarding their journey unless they invite you in. Avoid overly personal questions that might make them uncomfortable. Allow them to share at their own pace, try using open-ended questions such as, “Would you like to share more about how you’re feeling?” This approach empowers them to control their narrative while ensuring they feel supported.
Focus on Identity, Not Sexuality- Keep the conversation centered on their identity rather than sexual preferences or activities. Coming out is about identity, not just sexuality. Recognizing that sexual orientation and gender identity are fundamental to a person’s sense of self helps create a respectful and affirming environment.
Don’t Dismiss Their Experience- Avoid minimizing their journey with comments that suggest “it’s just a phase” or “that you always knew”. Such remarks can be dismissive and belittling. Instead, acknowledge the significance of their disclosure and affirm their feelings. Show genuine curiosity and empathy, asking how you can best support them during this time.
Steer Clear of Negativity- Even if you’re struggling with the news, refrain from expressing doubts or negative feelings in response to their coming out. Manage your emotions privately and don’t impose them on the person who is sharing with you. If needed, seek support from other allies or professionals to process your feelings, ensuring that you prioritize the emotional safety and well-being of the person who has confided in you, it most likely wasn't easy for them.
“Coming Out?” vs. “Letting In?”
Letting in is an intentional act—a way to invite others into our inner world. It’s about choosing whom to share our truth with, rather than feeling pressured to present a polished narrative of our identities. This process acknowledges that our experiences are complex and can't always be put into simple statements or singular moments. When we let others in, we exercise the power of choice. It’s a way to engage in meaningful relationships, allowing us to decide who deserves a glimpse of our authentic selves. This choice empowers us, giving us agency over our stories and how we share them. Opening up can profoundly affect our lives. It has the potential to foster closer relationships and build trust. Yet, we must weigh this against the risks involved. Being selective about whom we let in can protect us while still allowing us to cultivate meaningful connections.Ultimately, letting in is about creating space for ourselves and others. It’s an invitation to explore the complexities of our identities and relationships. By choosing to let in those who align with our needs for safety and comfort, we embark on a journey of authentic connection, one shared moment at a time.
Resources
Parents: Tips for supporting your LGBTQ+ child and yourself during the coming-out process
The Coming out Handbook- The Trevor Project
“Coming Out?” or “Letting In?”: Recasting the LGBTQ+ Narrative
“Coming Out?” vs. “Letting In?”: Living & Sharing Truth
Support Hotlines
The Trevor Project: (866) 488-7386
The LGBT National Hotline: (888) 843-4564
The Transgender Crisis Hotline: (877) 565-8860
National Suicide Prevention Lifeline: 988
Question Persuade Refer
READ FIRST: Suicide is a difficult topic for many to talk about. If you have lost someone to suicide or have been suicidal, you are welcome to skip to the QPR section for prevention training. If at any point reading you experience any extreme emotions, thoughts, or behaviors, please call or text 988 and talk with a trained professional.
The more awareness we bring to suicide, the less darkness it has. And the less darkness it has, the less power it holds. Talking about it is difficult. But not talking about it is dangerous and deadly. Learn to respond when your friend is in trouble. Learn to react when no one else can. Learn to be the light shining in someone else's darkness so that we can help people have power over their mental health.
Why are people suicidal?
Most individuals who have made a serious suicide attempt and survived don’t truly want to end their life. If they don’t want to end their life, this suggests that there must be underlying reasons. There are two main reasons that have been studied that influence suicidal behaviors: Pain and isolation. Pain can take form in multiple ways including guilt, shame, remorse, unworthiness, addictions, substance use, etc. Isolation, especially within the LGBTQ+ community can look like rejection, disowning from family members, or lack of community.
Three feelings have also been studied that when blended together, the likelihood of suicidal thoughts are very high.
When the person feels unlovable
When the problem feels unsolvable
When the pain has grown unbearable
Warning Signs
80-90% of people who have died by suicide indicated warning signs before taking their life. I often hear people who have lost someone to suicide say “I didn’t think it was that bad” or “I didn’t think they were really going to do it.” Pay attention. Some of these signs may be easy to dismiss as attention seeking. If someone is seeking attention in this way, they need help. Other signs can easily be missed. Suicide is preventable and it may only take one positive action to save a life. Please pay attention.
Direct Verbal Cues:
I wish I were dead
I’m going to end it all
If___ doesn’t happen, I’ll kill myself
Indirect Verbal Cues:
I just want out
I won't be around much longer
I’m tired of my life, I just can’t go on
People would be better off without me
Pretty soon, you won't have to worry about me
ASK if you are uncertain about the intentions behind these phrases such as “Tell me more about that” or “What makes you think that?”
Behavioral Cues:
Any previous suicide attempt
Acquiring a gun or stockpiling pills
Putting personal affairs in order. For example; Receiving a random phone call from a friend thanking you for being there for you in high school
Giving away prized possessions. For example; Your friend gave you his favorite watch
Sudden interest or disinterest in religion
Unexplained anger, aggression, or irritability
What is QPR?
QPR stands for Question, Persuade, and Refer. It is a tool used to reduce suicidal behaviors through practical and proven suicidal prevention training.
Question the person directly about suicide
The fact that you ask is more important than how you ask it. If you cannot ask for whatever reason, find someone who can. Ask with respect. Remember that their life is the most important issue at hand. This is not about you and your feelings. This is about them and their safety. Do not bring up politics or beliefs. Don’t criticize or belittle them for being suicidal. Your job is to ask the question, listen, and let them talk freely. If they do not want to talk in depth about their experience, leave this up to a trained professional.
Indirect: Have you been unhappy lately?
Direct: You seem really sad lately and you matter to me. When other people go through these things its not unusual to have thoughts of suicide. Are you having these thoughts?
Persuade the person to seek and accept help
Listen for protective factors. Examples of protector factors include family, friends, responsibilities, hobbies, important people, religion
Affirm protective factors. What are sources of hope for them? Get them to talk about anything that they care about and affirm it. This will bring them back to the present and give them control.
Script: “You have a dog? I didn't know you had a dog. What kind is he?” or “I didn’t know you played guitar. What kind of music do you like to play?’
Point them towards hope when you sense those emotions deescalating
Script: “I know you are going through a lot right now but it seems like you still have some things that you care about and people who matter to you. Maybe it’s worth staying alive for now.”
Listen and Affirm if the emotions are not deescalating
Refer the person to appropriate resources
Best option: Take the person directly to someone who can help and stay with them
Second option: getting a commitment from them to accept help, then making arrangements
Third option: getting a commitment to not attempt or complete suicide and give the person referral information
If this is a situation where there is a firearm or the person is agitated, call 911. Always put your safety first.
Myths:
Myth #1: No one can stop suicide, it is inevitable
Fact #1: If the person gets help, they may never be suicidal again. Almost any positive action may save a life
Myth #2: Confronting a person about suicide will increase their risk of suicide
Fact #2: Asking someone directly lowers anxiety, opens communication, and decreases risk
Myth #3: Only experts can prevent suicide
Fact #3: Anyone can help stop suicide. Almost any positive action may save a life
Myth #4: People who talk about suicide will not do it - they are looking for attention
Fact #4: If someone is so badly needing attention that they are talking about suicide, give them attention. Ignoring them increases their risk of pain and isolation
Resources for LGBTQ+
National Suicide Prevention Lifeline LGBTQ: Call (press 3) or text (Q) to 988
National Suicide Prevention Lifeline: Call or text 988
Network 180 Crisis Line: 616-336-3909
Arbor Circle: 616-451-3001
LGBT National Hotline: Call 888-843-8564
LGBT National Senior Hotline: Call 888-234-7243
The Trevor Project: Call (866-488-7386) or text (start) to 678-678
Trans Lifeline: Call (877-565-8860)
MI211: Call 844-875-9211 or text 898211
For more information regarding content, please visit:
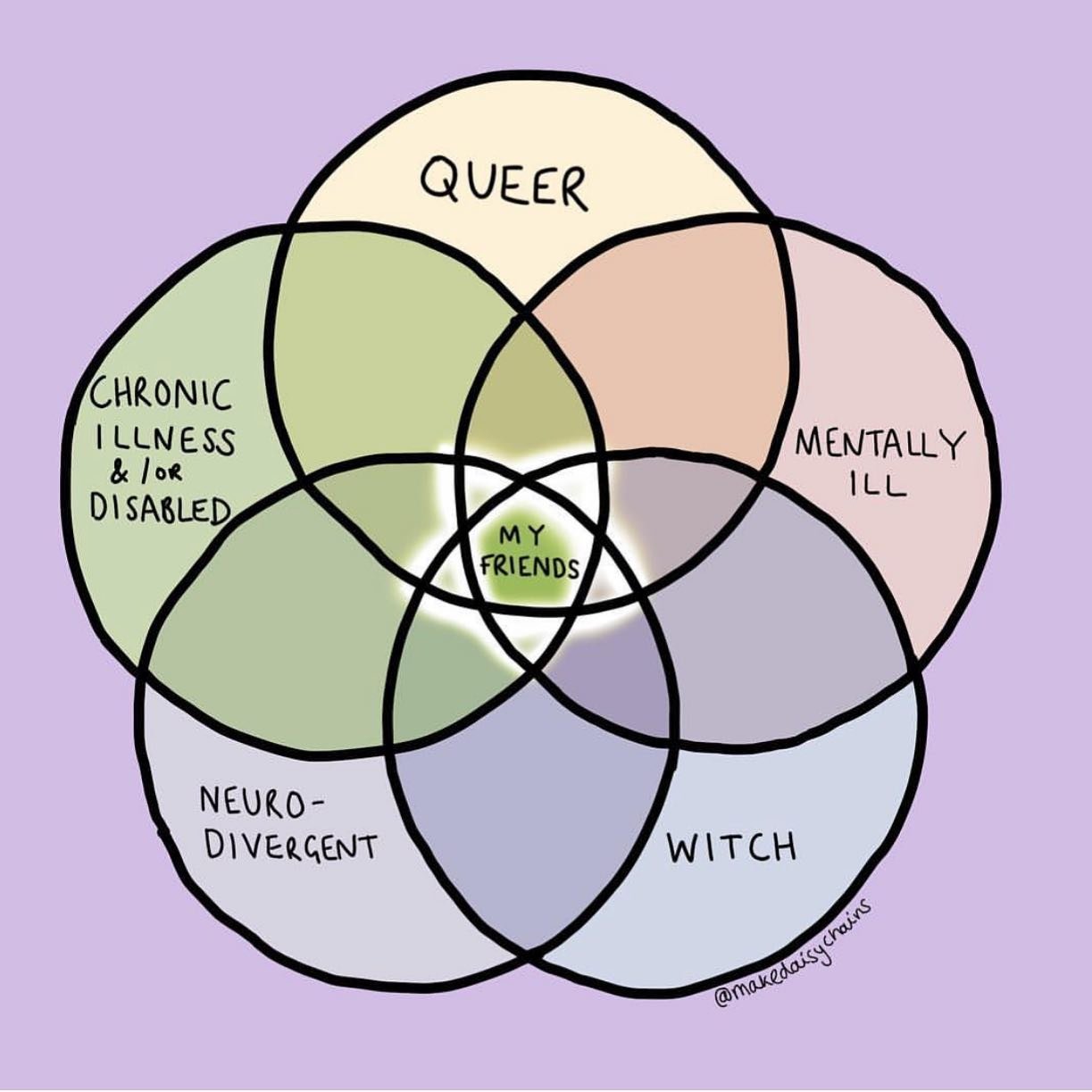
LGBTQ+, Disabilities, and Healthcare
While any LGBTQ+ community member can have any type of disability, one study from the Trevor project highlighted common disabilities among LGBTQ+ young people ages 13-24. In their study, nearly 1/3rd (29%) of LGBTQ+ young people identified as someone with a disability. Below are some statistics on the breakdown of these disabilities:
Mental Health Disorder: 72%
ADHD: 48%
Developmental/Learning Disorder: 32%
Physical Disability: 28%
Autoimmune Disorder: 10%
Oppositional Defiant Disorder: 3%
In comparison, 8% of the general population of young people ages 18-35 report having a disability. Cognitive disabilities were the most common at 10%. It’s important to note that research is still ongoing so these statistics may not fully be developed.
Access to healthcare has been a challenge for both LGBTQ+ people and people with disabilities. For people with disabilities, an inaccessibility to healthcare facilities, equipment, and transportation can be common. Additionally, healthcare professionals caring for people with disabilities may have knowledge gaps about language and specific healthcare needs. Similarly to people with disabilities, knowledge gaps may occur in healthcare professionals caring for the LGBTQ+ community. With these two intersectionalities, healthcare professionals should seek to learn how to best care for this community. Here are some examples of language usage for people with disabilities:
Use person first language. A person with disabilities is an individual before their disability. For example; say “a person who uses a wheelchair” instead of “wheelchair bound” or “a person with disabilities” vs “a disabled person.”
Use identity first language when preferred by the individual. This language is used as a reclamation of disability identity and indicates disability pride. It is most common for autistic people and people in the deaf community but can encompass other disabilities depending on the individual. For example; say “Autistic person” rather than “a person with autism.” Always ask before using identity first language.
Avoid ableist language such as “stupid,” “crazy,” “dumb,” “crippled,” “lame” or phrases such as “I’m OCD about…”
Having healthcare providers understanding and addressing healthcare gaps builds credibility with LGBTQ+ people with disabilities. One survey concluded that 72% of LGBTQ+ people with disabilities avoid discussing their LGBTQ+ identities with their healthcare providers with 9.8% never having disclosed their LGBTQ+ identities. Reasons indicated included negative interactions (fear, distrust, avoidance of care) at 40.1%, dismissal/denial of treatment at 30.5%, and assault/aggressive activity at 4.1%. It is important to disclose this information to a trusted healthcare provider, given that it is a safe space to do so, in order to keep in good health. Benefits of disclosing this information include caring for needs specific to identity, using preferred names/pronouns, and providing additional support for the individual or family members.
Here are some Action Steps for healthcare providers to help build trust:
Ensure that medical equipment is available to people with disabilities such as scales, examination tables, or chairs
Plan for additional time during exams
Communicate on the patients level wherever that may be. Make sure the person is understanding what you are saying. If you are unsure of what they are saying, repeat back what you heard
Always treat the person with a disability as an independent individual. If the person has someone with them for interpretation purposes, still speak directly to the person rather than the interpreter.
Don’t assume that they need help. Always ask before helping or initiating physical contact.
When addressing someone using a wheelchair or other mobility device, offer to shake hands as you would with anyone else and make eye contact at the person’s level.
Free Webinar
Trauma Informed Care
What is trauma?
“Trauma results from an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being” (SAMHSA, 2014, p. 72 ) In other words, trauma can be understood as any extraordinarily stressful experience in life that has a lasting negative impact on someone.
What is Trauma Informed Care?
A trauma-informed approach to the delivery of behavioral health services includes an understanding of trauma and an awareness of the impact it can have across settings, services, and populations. It involves viewing trauma through an ecological and cultural lens and recognizing that context plays a significant role in how individuals perceive and process traumatic events, whether acute or chronic. Trauma Informed care looks at the person as a whole instead of just physically or mentally.
The Neurobiology of Trauma
Trauma Informed care looks specifically at adaptation or how the nervous system is constantly adapting to how the nervous system responds. When an extraordinarily stressful event happens, the brain can store that information. When the event is over, your brain continues to react to the information as if you are still in danger. Brain areas implicated in the stress response include the amygdala, hippocampus, and prefrontal cortex. There are five types of stress responses which can vary depending on the person and situation. These types include:
Fight happens from the waste up. Muscles tense up and fists/jaws can clench. Feelings can include wanting to punch or yell in order to get out of the situation.
Flight happens from the waste down. Legs can be tense and muscles contract. Feelings can include wanting to run or having restless legs.
Freeze happens from head to foot. You can’t respond or move. From an evolutionary perspective, this is helpful to blend in with the surroundings
Fall happens when the body becomes physically or mentally unresponsive. Fainting may happen. From an evolutionary perspective, the body preserves energy
Fawn is the drive to appease the aggressor. This response happens in the prefrontal cortex because it takes a lot of thinking to not say the wrong thing
What does trauma in the LGBTQ+ community look like?
Trauma in the LGBTQ+ community is similar to trauma faced in other populations.The biggest difference is that it's magnified because not only is the bad thing happening but the bad thing is happening because of being LGBTQ+. Some common themes surrounding the LGBTQ+ community found among mental health therapists include:
Religious trauma
Conversion therapy
Stigma surrounding what a marriage should look like
Toxic relationships
Boundary crossing
Difficulty identifying toxic relationships
Family relationships
confusion around people who are “accepting” but not accepting
Toxic family dynamics
What does trauma informed care in a healthcare setting look like?
There are several domains in which the approach to Trauma Informed Care can be applied to. These domains include:
Safety (Physical, Psychological, Emotional)
Be aware of your body language with a patient – don’t tower over patients or visitors, allow a patient an option of where to sit in the room so that they may see and access the door.
Trustworthiness and Transparency
Let patients know which parts of the body may be impacted before beginning or proceeding with an exam. When possible, allow patients more control of care steps, i.e. apply gel, holding a stethoscope.
Collaboration and Mutuality
Learn about patient strengths and resources to manage past challenges. Ask “what has worked for you in the past?”
Empowerment, Voice, Choice
Provide options wherever possible: - Doors, curtains, shades – can the patient decide if they want those open or closed? - If a patient has to be woken up for meds or vitals, ask how they would prefer to be woken up. - Conduct as much of the visit with a patient’s own clothes on rather than dis-robing.
Recognition of Cultural, Historical and Gender Issues
Use interventions that respect diverse cultural backgrounds and create opportunities for patients to engage in culturally sensitive interventions and practices that promote trauma healing and recovery.
Peer Support
Promote healing and recovery by valuing lived experience of patients and individuals with shared experiences. For example, create mutual support groups for patients and offer peer supporters/navigators as part of health care delivery.
A full comprehensive list can be accessed here
Pride Month
Why do we celebrate pride?
Before Stonewall, "Reminder Day Pickets" took place in order to regain the rights to work for the government. Many LGBTQ+ people were fired due to their sexual orientation so silent protests were held every year in hopes to gain this right back. With oppression still continuing, a riot eventually broke out at the Stonewall Inn on June 28th, 1969. Protesting and riots continued for 6 more days. This served as a catalyst for the Gay Rights Movement. Yearly marches were then held to commemorate stonewall. Watch this video to learn more about the events leading up to Stonewall.
What does pride mean?
The word “pride” can be broken down into two different facets: Authentic and hubristic. Hubristic pride is defined as having an excessively high opinion of oneself with egoistic and arrogant characteristics. This type of pride is unhealthy because it is associated with aggression and relationship dissatisfaction. Authentic pride includes satisfaction taken in an achievement, possession, or association. This type of pride is the more common understanding in reference to pride month. Pride month is a commemoration of Stonewall and the progress of LGBTQ+ individuals. This is authentic pride because it involves a satisfaction of achievement and association to a larger group - and this is something to celebrate! For example; Someone may say “I am proud to be part of a community who values and respects who I am.” This is what pride month is all about - a celebration of authenticity, diversity, and togetherness.
Why is having pride important?
Authentic pride (in moderation) is very important. This type of pride can be healthy because it can encourage us to succeed and promote prosocial behaviors. In terms of mental health, pride can have many benefits including high self esteem, self worth, confidence, and sense of accomplishment. However, moderation is the key. One quote based off of Aristotle explains this:
“Too little is failing to acknowledge what has been achieved—a form of false humility—and too much is vanity.”
Pride Events:
Grand Rapids
Date: June 22
Learn more: Grand Rapids Pride Center
Detroit
Date: June 8-9
Learn more: Motor City Pride
Lansing
Date: June 22
Learn more: Lansing Pride
Holland
Date: June 29
Learn more: Out On The Lakeshore
Muskegon
Date: June 1 at 10:30
Learn more: Muskegon Pride
Grand Haven
Date: June 8
Learn more: Grand Haven Pride
Autistic Adults
How are autistic characteristics in adults different?
Autistic characteristics in adulthood may look differently than in childhood. Characteristics that are more common in adulthood may include:
Difficulty in understanding other people's thoughts or emotions
Anxiousness in social situations
Difficulty in making friends or preferring to be alone
Sounding blunt, rude, or uninterested in others without intending to
Difficulty in explaining feelings
Taking words or phrases literally
Having the same routine and feeling distressed if the routine is not followed
Other characteristics may include:
Not understanding social rules
Avoiding eye contact
Getting too close or getting upset if others get too close
Noticing details, patterns, smells, or sounds if people get too close
Having a keen interest in certain subjects or activities
Planning things before doing them
autism and queerness
The largest study on sexual activity, orientation, and health of autistic individuals reaffirms previous research that autistic individuals are more likely to have a wider range of sexual orientations than non-autistic individuals. The results from this study reveal that autistic people are 7-8 times more likely to identify as asexual or non-heterosexual orientations. It is not very understood as to why this is.
Words of the Autistic community:
Neurotypical - an informal term used to describe a person whose brain functions are considered usual or expected by society. (Rudy,
Neurodiverse - refers to differences in brain function among people diagnosed with an autism spectrum disorder (ASD)
Neurodivergent - describes someone who isn't neurotypical
Meltdown - Having extreme reactions to specific situations. When someone is overstimulated, they may lose behavioral control. This can look like crying, shouting, laying on the floor, and sometimes engaging in dangerous behaviors such as self-injury or aggression.
Sensory Processing - sensory problems relating to sights, sounds, smells, taste, touch, balance, and general body awareness. There are two types of sensory processing: Hypersensitivity (over-responsiveness) and hyposensitivity (under-responsiveness).
Stimming (self-stimulatory behavior)- specific, repetitive behaviors that can include hand-flapping, rocking, spinning or repetition of words and phrases
Preservation - repetitive or persistent action or thought, after the stimulus that prompted it has ceased. The person may have difficulty shifting gears.
Masking - camouflaging autistic characteristics
For more words, click here
Autistic Assessments:
If you think you might be autistic, talk to your doctor or therapist if you would like to receive an Autism Assessment. An assessment may help you to understand why you might find some things harder than other people, explain to others why you see and feel the world in a different way, and get support at college, university or get some financial benefits. Before your assessment, Here are some ways you can prepare:
Write a list of the signs of autism you think you have and bring it with you
Ask people who know you if they have noticed any possible signs
If helpful, bring someone with you who knows you well
Purple Ella
Purple Ella is Autistic, ADHD, nonbinary, content creator, and advocate. Check out their video about their experience with the Adult Autism Assessment:
Empowering Survivors of Domestic Violence
What is Domestic Violence?
Domestic violence is defined as “a pattern of abusive behavior that is used by an intimate partner to gain or maintain power and control over the other intimate partner” (Domestic and Dating Violence, n.d). It can be any action that is physical, sexual, emotional, economic, or psychological. Behavioral intentions can be to intimidate, manipulate, humiliate, isolate, frighten, terrorize, coerce, threaten, blame, hurt, injure, or wound someone.
Domestic Violence in the LGBTQ+ Community
Domestic Violence in the LGBTQ+ community can be experienced at the same rate in similar ways as non-LGBQT+ people. However, different obstacles may impact the LGBTQ+ community.
Fear of Isolation - many community members belong to families with traditional values, oppressive living environments, or religious communities. The abuser may use this isolation and have the person be more dependent on them
Shame of Identity - the abuser may play into the person's internalized homophobia and shame them for their pronouns or chosen name. The abuser will use power and control to keep the person in isolation
Fear of not receiving services - In the LGBTQ+ community, minimization of domestic abuse can happen meaning that others might not view domestic abuse in the LGBTQ+ community as legit.
Variation of legal protection - receiving legal resources for domestic violence can vary depending on the state. Impact and state reports can be found here.
What to do if you know of someone experiencing Domestic Violence
If you know of someone who is in a domestic violence situation, it’s important to consider the wants and needs of the person in the situation. They may or may not have acknowledged that they are in a bad situation. Until they acknowledge this and want help, honoring their wishes and boundaries is important in establishing yourself as a safe person. Below are several steps you can take to help:
Ask them what they want - Is there some way you can support them?
Document the abuse every time you hear about it
Create a safety plan with the person experiencing abuse if they are ready
Knock on their door to make an excuse of why you are there as a way to interrupt whatever is happening
“I just ran out of eggs. Do you have any I can use?”
Reach out to the YWCA if you need additional support
Call: (616) 454-9922
Location: 25 Sheldon Avenue SE Grand Rapids MI, 49503
How the YWCA is addressing Domestic Violence
Jenna Schook, the Volunteer Advocate Program Manager, enjoys connecting with survivors when they come in. The YWCA provides services for survivors of domestic violence and dating abuse. The organization is unique in having a Nurse Examiner Program that provides medical forensic exams at no cost.
When a survivor reaches out to the YWCA, they will first talk to a nurse to schedule an exam. During the appointment, they will meet with an advocate (emotional supporter) and nurse while talking over any questions or concerns. A survivor has control over how the exam will go. Nothing is going to happen without the consent of the survivor. If the survivor chooses to give consent to having the full exam, the following steps will take place:
History about the details of the assault or abuse that took place
Physical exam
Discussion over possible medications, safety planning, or different resources
Volunteer with the YWCA
Volunteer Advocates are people who walk alongside survivors throughout the entire process. While anyone who is interested in being a volunteer is encouraged to reach out to the YWCA, volunteers within the LGBTQ+ community are needed. Volunteers within the reflected communities can experience a special connection with survivors that those outside of these communities cannot make. Additional healing and comfort can arise from survivors being matched with someone who reflects their unique identity.
Some essential duties for volunteer advocates include answering helpline referrals when a sexual assault call is made and being in the exam room with the survivor when the nurse calls. Volunteers can generally expect to be on call for one 12 hour shift. Around the holidays, volunteers can expect two 12 hour shifts. If you are interested in being a volunteer, reach out to Jenna Schook at jschook@ywcawcmi.org or go to the YWCA website and fill out an application.
Lgbtq+ specific Resources
Domestic Abuse and its impact on Transgender and Nonbinary Survivors
LGBTQ+ Sexual Violence Prevention and Response Toolkit
Am i experiencing domestic violence
Cervical Cancer Awareness
What is Cervical Cancer?
Cervical cancer is cancer that starts in the cells of the cervix. First, abnormal cells appear in the cervix and go through a process called dysplasia. If left untreated, the cells develop over time and become cancerous, potentially infecting the surrounding area.
What does screening look like?
Depending on the age group, screening is highly encouraged for people with a cervix every 3-5 years. During screening, a pap test is used to collect cells from the cervix which are then examined to determine if the cells are cancerous. Since anxiety is common with these types of exams, options such as being put under or a self pap may be offered.
Concerns about the LGBTQ+ community relating to care
There are many concerns regarding healthcare experiences within the LGBTQ+ community. Suzanne West, an OBGYN, is an affirming provider in the Grand Rapids area who voiced her concern. Her primary concern is that the community is at greater risk for cervical cancer due to the avoidance of care. When screening for cervical cancer becomes a regular routine, cervical cancer is 100% preventable. In fact, cervical cancer screening decreases death by 50%. If the avoidance of care remains unaddressed, the LGBTQ+ community will continue to be at an increased risk. This will have to be a community effort to better educate and equip our healthcare professionals in their understanding of LGBTQ+ Identities.
Why do LGBTQ+ community members tend to avoid care?
According to one study, 1 in 6 LGBTQ+ individuals reported avoidance of healthcare due to anticipated discrimination. To gain insight as to why this is, Suzanne West was asked this question. When asked this question, she stated a couple of reasons for the tendency to avoid care:
Negative experiences or poor treatment from healthcare workers
LGBQ: 6% of health care providers refused to see them due to sexual orientation
Transgender: 29% of health care providers refused to see them due to gender identity
2. Lack of financial support
44% of LGBTQ+ people ages 18-64 were earning less than $13,590 (per individual) per year in 2022. That’s 200% of the federal poverty level
How can healthcare providers adapt to the language for them to feel comfortable?
Healthcare providers can decrease negative experiences with healthcare by adapting the language that is used with patients. For people who have a different gender identity, using less gendered terms may reduce fear. Below are some tips on how language can be addressed:
Use less gendered terms
Example: “Exam” rather than “Vaginal Exam”
Ask: What language would you like me to use to describe your results?
2. Remove fear of the exam
Show equipment used
Communicate simple explanations
3. Use proper names and pronouns
Double-check forms to ensure accuracy
4. Educate yourself about LGBTQ+ language
LGBTQ+ Youth: Unsheltered and Unstable housing
Note: the term “unhoused” is sometimes used in replacement of “homeless.”
According to multiple sources, LGBTQ+ youth are disproportionately impacted by homelessness (Choi, Wilson, Shelton, & Gates, 2015; Durso & Gates, 2012; Morton, et al., 2018; Baams et al., 2019). True Colors United estimates that 7% of US youth are LGBTQ+ while 40% of LGBTQ+ youth are unhoused. This proportion means that LGBTQ+ youth are nearly five times more likely to experience unstable housing or homelessness than the general population. There are four main factors contributing to this overrepresentation:
Family Conflict
According to The Trevor Project, 14% of LGBTQ+ youth were kicked out or abandoned. 40% of those instances were due to sexual orientation or gender identity. 16% of LGBTQ+ youth ran away. 55% of those instances were due to mistreatment or fear of mistreatment due to sexual orientation or gender identity.
Aging out of Foster Care
LGBTQ+ youth who reported past housing instability or are currently unhoused had nearly 6 times greater odds of reporting that they had been in foster care at any point in their lives.
Poverty
Overall, the LGBTQ+ community is more likely to experience poverty than cisgender and heterosexual people. Looking at data from 2020, 23% of LGBT people lived in poverty compared to 16% of non-LGBT people.
Shortages of Shelters and Housing Programs
On any given night in Michigan, there are 8,206 people who are unhoused. While there are 184 homeless shelters in Michigan, there would have to be about 45 open beds in each of these shelters to house all of these people.
Watch this video to learn more about LGBTQ+ youth who are unhoused and how you personally can make an impact.
While many policies in Michigan have been put into place for LGBTQ+ acceptance, there is still much work to be done across the US. Policy change against systematic oppression is needed in order to eliminate youth who are unhoused in the LGBTQ+ community. Here are some recommendations from Mel Moore, an activist, on how policy can help eliminate barriers:
Social support instead of criminalization for life sustaining activities out in public. According to the National Coalition for the Homeless, criminalization activities may include:
Confiscating personal property (tents, bedding, medications etc.)
Criminalization of panhandling (begging for money)
Criminalization for publicly sharing food with the homeless
Enforcing a “quality of life” ordinance relating to hygiene
Research suggests that 48 states in the US has at least one law criminalizing homelessness activities. If we truly want homelessness to be resolved, a focus should be placed on how to provide housing and stability rather than criminalization of life sustaining activities.
Ban conversion therapy in all states. Currently, 22 states have a ban on conversion therapy. Conversion therapy is the attempt to change one’s sexual orientation to straight or one’s gender identity to cisgender. Studies have not shown conversion therapy to be effective but have proven this therapy to be very harmful. Watch this video to learn more about conversion therapy. Conversion therapy can contribute to family conflict, which can lead to further stigmatization and unsafe home environments.
Support organizations that advocate for policy change to end homelessness at the local, state, or global level. Below are a list of advocacy organizations:
Kent County: Coalition to End Homelessness
Michigan: Michigan Coalition Against Homelessness
United States: National Coalition for the Homeless National Runaway Safeline
LGBTQ+ Specific: True Colors United Chosen Family of West Michigan
Resources
How can I help?
Do you need help?
National Homeless Shelter Directory
Locate a Homeless Youth Shelter
Concerned Adults
Service providers
Intersex Identities
The term Intersex refers to a person who has variations of male and female physical, hormonal, or genetic sex traits which can appear at birth or later in life. Intersex people are estimated to be born in approximately 2% of live births.
There is much debate over the ethical practice of surgical intervention for intersex infants. Historically, intersex individuals have been considered “abnormal” and in need of fixing regardless of whether or not the treatment was medically needed. This idea stemmed from John Hopkins University in 1950 when they introduced the “Optimum Gender of Rearing Model.” With this model, typical gender upbringing was emphasized and genital surgeries were highly encouraged for intersex infants. According to the American Academy of Family Physicians, genital surgeries should only be recommended if it “[resolves] significant functional impairment or reducing imminent and substantial risk of developing a health- or life-threatening condition.” While surgeries are necessary in some cases, it’s critical to acknowledge the potentially harmful impacts that medically unnecessary surgery can have. It’s important to take note that forgoing unnecessary medical surgeries on infants have no evidence of having psychosocial problems later in life. Especially since the intersex individual can choose to receive these surgeries when they are old enough to consent. Surgeries impacting the genitalia may have negative irreversible effects such as “infertility, chronic pain, inaccurate sex/gender assignment, patient dissatisfaction, sexual dysfunction, mental health conditions, and surgical complications.” One medical personnel shares their insights:
“They [intersex people] get tired [of the entire situation]. Generally, when we see them here it is for another reason or for a complication. They are patients who have been seen and treated many times. They are not coming for a follow up. They don’t want to know anything. They’ve had surgeries, disorders of their sexuality. They don’t have a sex life. They’re not interested because there’s pain, they don’t feel much pleasure, and also because of the surgeries, which are not harmless: they cause adhesions or scar-like tissue, they have abnormal wound healing and [result in] many complications… they don't end up the same.” (Interview 5: medical personnel)
Further supporting this insight, The World Health Organization, American Academy of Pediatrics, twelve United Nations agencies, and several other organizations denounced early genital surgeries from 2010-2017. Although several organizations highly discourage this practice, medically unnecessary genital surgeries are still legal today in the US and may be practiced by medical professionals. Watch this video about how these irreversible surgeries impact the lives of children and their surrounding loved ones.
Resources
for the intersex community
Seeking Medical Care as an Intersex Person
For parents of intersex children
How To Retrieve Medical Records
Know Your Rights: A guide for parents
for medical providers
Ethical Guidelines for Intersex Surgeries
Intersex Affirming Hospital Policies
Affirming Primary Care for Intersex People
advocacy and support groups
learn more about the intersex community
The Do’s and Don’ts of Being an Ally
Watch Every Body Movie trailer
Read XOXY: A Memoir (Intersex, Woman, Mother, Activist) by Kimberly Zieselman
Legislative Toolkit: How to create change in your state
LGBTQ+ US Military History
History reveals where we have walked and where we have yet to travel. LGBTQ+ people have stumbled over rocks and trudged through mud all while dodging tree branches that seemingly never fail to swing towards them. LGBTQ+ military folks in particular may be familiar with these kinds of struggles, not only from bootcamp, but by oppression from the military throughout history. With currently 6.1% or 1.3 million LGBTQ+ members serving in the military, various policies have impacted the environment for those serving.
Check out this timeline of LGBTQ+ US military history overview as we conclude LGBTQ+ History Month and approach Veterans Day this November.
1953
Executive Order 10450 implied the ban of LGBTQ+ people in the military by using the phrase “sexual perversion.” The phrase “sexual perversion” was used to describe those who were not allowed to be employed by the government which led to 7-10,000 lost jobs. The number of people released from service due to sexual orientation is unknown.
1982
A Department of Defense policy was enacted stating that “Homosexuality is incompatible with military service.” This policy prohibited service for those who “engages in, desires to engage in, or intends to engage in homosexual acts.” This was a more specific ban on LGB people most likely due to an increase in community awareness of the LGBTQ+ movement.
1993
The Don’t Ask Don’t Tell Policy was enacted which allowed gay, lesbian, and bisexual people from serving as long as their identity remained unrevealed. It is estimated that between 14,000-43,362 of gay, lesbian, and bisexual people were discharged from the military due to this policy. Factors such as fear, imbalance of power, retaliation, and trauma likely influenced this wider range.
2011
The Don’t Ask Don’t Tell Policy was repealed through former president Barack Obama. Gays, lesbians, and bisexuals were able to serve openly in the military. Although the repeal was a great start, there was still a lot of progress to be made with homophobia in the military. Watch how this policy impacted the LGB population.
2013
The Department of Defense implemented Survivor Benefit Coverage to same-sex spouses of military members and veterans. Official document explaining benefits can be found here.
2016
Transgender people are finally able to serve… well kind of. For all transgender people with no diagnosis of gender dysphoria, they were allowed to serve only in their sex assigned at birth. For current service members, they were only able to serve if fully transitioned. For new applicants with a diagnosis or history of gender dysphoria, or if they had a history of medical transition treatment, they were only allowed to serve if they had been transitioned for 18 months. The reasoning behind the specific rules involves physical transitioning may involve more extensive accommodations than the government was able to provide. For further clarification, see this chart. This content may contain culturally inappropriate language.
2018
Enacted by former President Trump, transgender people were banned from the military unless they were diagnosed with gender dysphoria before 2018 and/or willing to stay in their sex assigned at birth. This meant that anyone who was in transition, who had transitioned, or who was “unstable” in their sex assigned at birth could not be in the military. This ban impacted thousands of transgender people already in the military. Watch how the impending band impacted military members.
2021
The transgender ban was reversed by president Biden allowing transgender individuals and those with gender dysphoria to serve openly in the military. The following provisions were added:
The military provides a process for people to transition while serving
A service member may not be discharged due to gender identity
The military has a procedure for changing a service member’s gender marker
Veteran Healthcare Resources
How to add/change gender or name on va.gov
Veteran Sexual Health and Sexual Orientation
Veteran Health Care for Gay, Bisexual, and Queer Men
Veteran Health Care for Lesbian, Bisexual, and Queer Women
Veteran Health Care for Transgender and Transmasculine Men
Provider Resources for LGBTQ+ Veterans
Veterans Health Administration LGBTQ+ Training
CDC TRAIN: LGB Veteran Health Care
CDC TRAIN: Transgender: Older Transgender and Gender Diverse Veteran Care
CDC TRAIN: Transgender: Care for the Gender Nonbinary Veteran
CDC TRAIN: LGB Sexual Health Care for Genderqueer and Nonbinary Veterans
CDC TRAIN: Healthcare Concerns for Older LGB Veterans
The Overlap of Neurodiversity and Queerness
April is Autism Acceptance Month, so for this month’s blog we want to explore the intersection of LGBTQ+ and neurodiversity more generally. In addition, we’re going to share some tips for providers and healthcare professionals on caring for, treating, and plain ol’ interacting with neurodiverse LGBTQ+ patients. Much like other marginalized groups, neurodiverse LGBTQ+ people face unique barriers to care and suffer due to misinformation, discrimination, and medical mistrust. In order to go beyond awareness of Autism and neurodiversity towards acceptance, we must continue learning how to be affirming allies and break down misinformation.
What does neurodiverse mean?
According to Neurodiversityhub.org, “Neurodiversity refers to the virtually infinite neuro-cognitive variability within Earth’s human population. It points to the fact that every human has a unique nervous system with a unique combination of abilities and needs.” Much like how “LGBTQ+” houses a variety of identities under its umbrella, the term neurodiversity covers a variety of neurotypes and variations of the human mind. The neurodiverse umbrella includes Autism Spectrum Disorder (ASD), Attention Deficit Hyperactivity Disorder (ADHD), sensory processing disorders, tic disorders, and many others.
What is ableism?
Ableism is a system of oppression that operates on the belief that able-bodied, neurotypical people are the norm, that disabled, neurodiverse people are abnormal and are therefore discriminated against. According to the Therapist Neurodiversity Collective, “Ableism is entrenched in the presumption that neurodivergent and/or disabled people are "broken" and need to be ‘fixed.’”
[image description: a digital illustration of a Venn diagram which consists of 5 circles which overlap in the center. In the middle it says “my friends”. The other 5 circles each have one of the following written in it clockwise : queer, mentally ill, witch, neurodivergent and chronically ill &/or disabled”. In the middle where it says “my friends” there is a hidden glowing pentagram. The background is lilac. ]
The way that we’ve grown to understand neurodiversity, as well as the spectrums of sexual orientation and gender identity, has allowed more and more people to share their experiences and for the topic to gain attention from researchers. In a study published in 2022, researchers found that “autistic people self-reported lower quality healthcare than others across 50 out of 51 items.” The study also found higher rates of a variety of chronic physical and mental health conditions, ranging from arthritis and insomnia to anxiety and depression. In addition, LGBTQ-identifying patients are at higher risk of anxiety and depression, as well as STIs and substance use. While there is still more research that needs to be done on the intersection of neurodiversity, queer identities, and gender diversity, there is evidence that supports the community observation of higher rates of autism and neurodiversity in queer and trans spaces. According to National LGBT Health Education Center,
“Evidence suggests that neurodiverse people, particularly those on the autism spectrum, are more likely to be gender diverse and have a lesbian, gay, bisexual, queer, or asexual sexual orientation, compared to neurotypical people. The reasons why are not well understood. One possibility is that neurodiverse people tend to be less aware of, or less susceptible to, societal pressures and gender norms; therefore, they can express their gender identity or sexual orientation without concerns of being judged or fitting into certain roles.”
This intersection of identities can create added stress in non-affirming environments, leading neurodiverse LGBTQ+ patients to avoid receiving care, even when they need it. Acceptance for both neurodiverse and LGBTQ+ folks still has a long way to go, but there are steps that providers and healthcare workers can take to support their neurodiverse, LGBTQ+ patients.
First and foremost, listen to what the patient has to say about their identity and be affirming. Implying (or flat out saying) that a neurodiverse patient may not actually be their identity because it’s a “special interest” or that they aren’t able to properly articulate their feelings is disheartening and even damaging.
Talk with the patient about the terms and labels that they use to describe themselves (if any). Trust that the patient knows themselves better than you or anyone else can, and that their perception of self may not line up with traditional ideas.
Ask direct questions about partners, health, and other important information, as neurodiverse folks are less likely to fill in the gaps themselves.
Want to learn more about neurodiverse identities and their intersections with the LGBTQ+ community? Check out the links below!
Neurodiversity & Gender-Diverse Youth: An Affirming Approach to Care
Neurodivergence as Queerness · Public Neurodiversity Support Center
Reporting Healthcare discrimination and bad experiences
In the LGBTQ+ community, it is not uncommon for folks to avoid going to the doctor, whether due to previous bad experiences, fear of coming out or being outed, medical mistrust, or just not sure where to start. In fact, in the Grand Rapids LGBTQ+ Healthcare Consortium’s 2022 survey on LGBTQ+ patient experiences, nearly 57% of respondents stated at least one reason for avoiding healthcare over the last year. In addition, of the 39 respondents who have avoided receiving care due to fear of discrimination from front desk staff/provider and/or general transphobia, 32 (82%) stated experiencing microaggression, discrimination, prejudice, or other stigmatization. So it’s fair to say that the fears and mistrust among the community are well founded and valid. But what do you do if you experience discrimination or have a negative experience while receiving care? Is there anything you can do?
That’s what we’ll be answering in this blog, in honor of LGBT Health Awareness Week, which aims to bring attention to the devastating cycle of discrimination and health disparities that affects the lesbian, gay, bisexual and transgender (LGBT) community (according to the National LGBTQ Task Force). Because LGBT people are regularly discriminated against in employment, relationship recognition and insurance coverage, they are more likely to get sick and less likely to be able to afford vital health care than their straight and non-transgender neighbors. One last note, as a heads up, we do use some legal jargon and site laws in the blog, but will do our best to summarize the main points; we want to ensure that if folks want to do further research or have questions, you have the points of reference for what we’re talking about.
First off: are LGBTQ+ protected under Michigan Law from healthcare and insurance discrimination? Yes, actually: any facility, provider, clinic, agency, or other entity that accepts Medicaid, Medicare, or otherwise receives federal funding cannot deny care or service to someone because of their race, color, national origin, sex, gender identification, sexual orientation, age, or disability. This also goes for private insurers as well, according to a March 2022 bulletin from the Michigan Department of Insurance and Financial Services.
So we’re legally protected from discrimination; what happens if you experience discrimination and need to file a complaint? In Michigan, any hospital that accepts Medicaid/Medicare has to have a patient relations department, and “are to ensure compliance with all relevant Federal and State nondiscrimination provisions,” (MDHHS Medicaid Provider Manual, pg 14).
It can be pretty daunting and draining to seek help after a negative experience, especially when you’re not sure if you’ll be safe making the report. But letting discrimination go unchecked allows the cycle to continue, with the possibility of more medical mistrust and care avoidance in the future. Below is a general list of what you’ll need to submit the complaint, as well as links to 6 community healthcare organizations, 2 Michigan departments, and Legal Aid of West Michigan, should you need to take legal action.
What you’ll need:
The date of the incident
What occurred and by whom
The address of the organization
Trinity Health Patient Relations
Corewell Health Compliments and Complaints
University of Michigan Health West Patient Relations
Catherine’s Health Center Contact Form
MDHHS Bureau of Community and Health Systems
To dive a little deeper into legal protections: while the protections under Section 1557 of the Affordable Care Act were (briefly) removed in 2020, they were restored in 2021 by executive order. Policies and laws that prohibit discrimination on the basis of sex include gender identity and sexual orientation in their definition, according to the order. In the MDHHS Medicaid Provider Manual, it states that “an individual shall not be excluded from participation in, be denied the benefits of, or be subjected to discrimination on the grounds [of race, color, national origin, sex, gender identification, sexual orientation, age, or disability] under any health program or activity, any part of which is receiving federal financial assistance, or under any program or activity that is administered by an Executive Agency or any entity established under Title I of the Affordable Care Act or its amendments.” In addition, we are protected under the Michigan Public Health Code 333.20201:
(a) A patient or resident shall not be denied appropriate care on the basis of race, religion, color, national origin, sex, age, disability, marital status, sexual preference, or source of payment.
It’s fair to say that LGBTQ+ patients are legally protected from discrimination in a healthcare environment in a variety of ways, but we understand that folks still can (and do) experience discrimination, prejudice, and other stigmatization while seeking care. At the end of the day, it’s important to remember that you are entitled to quality, affirming care and should not have to endure discrimination and prejudice in order to take care of yourself and your health. We must empower ourselves to stop others from experiencing discrimination and from it happening all together. It’s okay to feel nervous, apprehensive, or scared about reporting discrimination, that is a perfectly normal reaction. If need be, ask a friend for support; you don’t have to go at it alone.
Note: we are not legal experts or lawyers, this is all general information to help get you started in reporting discrimination and knowing your rights.
Still Important, just not Romantic
Looking beyond Monogamous, Romantic relationships and the importance of Recognizing significant friendships & Other relationship structures - in honor of AroSpec Awareness week
Graphic made by Arly using Canva, AroAce flag made by aroaesflags
Following Valentines’ Day on February 14th, the 19th-25th is Aromantic Spectrum Awareness Week, a time to spread awareness and acceptance of aromantic spectrum identities and the issues arospec people face, as well as promoting awareness of the existence of arospec folks and celebrating them. As acceptance for non-cishet identities grows, so should the way we view relationships and support networks, expanding beyond monogamous, romantic relationships and biological families.
In the United States, according to the US Government Accountability Office (GAO), there are 1,138 federal statutory provisions where one’s marital status plays a role in determining benefits, rights, and privileges. Same-sex marriage is now included in these provisions, which is seen as a win for LGBTQ rights all across the US. But as we begin to view the myriad of ways that folks can form significant relationships outside of marriage, we can see how marriage is not the end-all-be-all of LGBTQ rights, especially from a patient rights lens. In this blog, we are going to explore a few ways that folks form relationships outside of marriage and why it is incredibly important for providers, other healthcare workers, and society at large to honor these relationships when it comes to medical decision making and support.
To start off, let’s talk more about aromantic and aro spectrum identities. According to aromanticism.org, the term “aromantic” (aro for short) describes someone who experiences little to no romantic attraction. Aromantic people are not broken, mistaken, or “waiting for the right person” and are still capable of establishing significant relationships outside of romance. For example, someone who is aromantic can also be allosexual, someone who experiences sexual attraction. Therefore, from a healthcare perspective, it would still be important to ask the patient whether they are sexually active, the type of sex they are engaging in, number of partners, contraception used, etc. Being educated on the terms that patients can identify as takes the burden of educating the provider off the patient, which is often tiring and stressful for the patient.
As noted previously, romantic attraction is on a spectrum; the way that someone views their identity and forms relationships can exist anywhere along not just the aro spectrum but also the asexual and aplatonic spectrums. If you’re getting a little overwhelmed here with all the spectrums, that’s okay, but it just shows that relationships can form and be experienced in ways far beyond our traditional understandings! With these expanding understandings of romantic, sexual, and platonic attractions, we can begin to see why holding marriage as the ultimate union doesn’t work for some folks.
Graphic made by Columbiaces
This idea of separate forms of attraction is known as the Split Attraction Model (SAM), which you can learn more about here. For some folks, the SAM doesn’t really work for them, whether they don’t relate to the language, find it too confusing, or just aren’t a fan of it (learn more here). No matter how someone defines their identity or what labels they use, we must trust that they know themselves better than we possibly could, while also acknowledging that labels can change.
For a great number of LGBTQ+ folks, they don’t have a biological family to rely on for support, which is where found/chosen family comes into play. Whether it’s a young queer teen in need of housing or an elderly trans person in need of home care, found family often provides needed support to survive after facing rejection from one’s biological family. This network of found family should be seen as just as valid as a biological family, as it provides the much needed love, care, and support that may not be guaranteed in one’s biological family. However, laws governing medical decision-making are mainly based on biological and marital relationships (part of the 1,138 federal statutory provisions mentioned above), leading to difficult, even complicated, situations for LGBTQ+ patients without advanced healthcare directives or other documents naming their found family to make decisions on their behalf.
I personally use a wide variety of labels to describe my varied places on the attraction spectrums, as well as my gender identity: pan/demisexual, greyromantic, polyamorous, transgender and non-binary. My parents are not involved in my life and my extended family is supportive but religious with differing views than mine on healthcare; my brother just became a legal adult and is navigating that special brand of chaos; I am not in any significant relationships at the moment; my main supports are my found family of older enbies and fellow Gen Z queers. So where does this leave me should I become unable to make medical decisions for myself? This is a question that myself and many other LGBTQ+ folks are left to ponder -and occasionally, are forced to scramble for answers.Our first pick to be our medical advocate may be unable to do so without proper planning and paperwork beforehand; our (disapproving) families may be the ones who come to our side because they are the only ones allowed to, leading to misgendering, deadnaming, and discriminatory care.
Holding marriage as the highest ideal to aspire to excludes the wide breadth of relationships that we can develop. Relying on only biological or legal families excludes the people in our lives that we hold just as near and dear to our hearts. Having significant relationships outside of romance and/or sex are just as valid and important; aromantics can still desire close relationships and be sexually active. Collecting sexual orientation and gender identity (SOGI) data is not just for data's sake: it is so that providers and healthcare staff can provide culturally appropriate care for their patients and ask relevant questions tailored to each patient’s needs. Medical mistrust and avoidance among the LGBTQ+ community due to discrimination and prejudice (anticipated or past experiences) means that preventable and treatable issues go untreated, leading to poor physical and mental health. Respecting the patient/person, as well as the terms and labels they use to describe themselves is a way to support mental and physical health; by fostering an affirmative, caring, trauma-informed environment, patients can feel comfortable enough to receive the care they need.
If you’d like to learn more about aromantic spectrum and other identities, check out the videos linked throughout the blog.
Cervical Cancer Awareness Month
January is Cervical Cancer Awareness Month, an opportunity to learn about cervical cancer, early detection, and HPV; the color teal is used to represent cervical cancer awareness. Cervical cancer and other gynecologic cancers are often talked about as a womens’ issue, which excludes transgender men and non-binary people. However, anyone who has a cervix can be at risk for cervical cancer, so it is important to stay up-to-date on screenings and vaccinations, as well as practicing safe sex practices in order to minimize one’s risk for cervical cancer.
According to the CDC, the main cause of cervical cancer is long-lasting infection with certain kinds of HPV, or human papillomavirus (not to be confused with HIV or human immunodeficiency virus). HPV is the most common STD in the US, according to the CDC, with an estimated 42.5 million people estimated to have it in 2018; it is spread by having vaginal, anal, or oral sex as well as close skin-to-skin touching during sex with someone who has HPV. While in most cases, HPV does go away on its own within two years, it can sometimes lead to health problems like genital warts (small bump(s) in the genital area) or cancer. Almost all cervical cancers are caused by HPV, so it is critical to be vaccinated against it as a preventative measure. The HPV vaccine, administered in two doses, is recommended for children ages 11-12 years, though it can be administered as early as 9 years old and as late as 26 years old, so talk with a medical professional about best steps for you/your child.
In addition to the HPV vaccine, screening tests are a vital preventative measure. Dr. Monique Small, CBHA obstetrician/gynecologist, says that “cervical cancer is one of the easiest gynecological cancers to prevent with regular screening tests.” It is recommended that people with cervixes begin getting Pap tests at 21 years old and every 3 years after, then begin HPV tests at 30 years old. A Pap test screens for abnormal, precancerous cells, which can be the first sign of cancer that develops years down the line. An HPV test screens for presence of HPV in cervical cells.
A common misconception is that LGBTQ+ people with cervixes don’t need to be screened for cervical cancer, but that is not the case. Anyone with a cervix should begin screening at 21 years old, no matter their gender identity or sexual orientation. As mentioned previously, screening is a vital part of catching cervical cancer before it grows and can spread to other areas like the vagina, bladder, rectum, or other nearby tissues.
Below are action steps to help lessen your risk for HPV and cervical cancer:
Talk with your healthcare provider about receiving the HPV vaccine
Use condoms, dental dams, and other safe sex practices
Get screened for cervical cancer, starting at age 21
Look out for genital warts, as this can be a sign of infection
If you are in need of an affirming provider to talk to about the HPV vaccine, getting screened for cervical cancer, or general preventative care, check out our provider directory for a list of affirming providers in the area. You can get free condoms and other resources at the Red Project, the Grand Rapids Pride Center, and Milton E. Ford LGBT Resource Center on GVSU’s Allendale Campus. It is important to take care of your health, as well as remember that you are not alone.
An Interview with a Gender Care physician
For LGBTQ+ patients, having to explain your identity or even stay in the closet during an appointment can be extremely draining and even dangerous. Having effective, affirming allies in healthcare is one way to lessen the burden placed on marginalized communities, for both patients and providers alike. But how can one be an ally in the healthcare environment? We asked Dr. Lisa Lowery about what allyship means to her, how she learns from mistakes, and her work at Helen DeVos Children’s Hospital Gender Care Clinic.
Arly: What does being an ally to the LGBTQ+ community in a healthcare setting look like to you?
Dr. Lowery: For me, being an ally means providing comprehensive gender affirming care while meeting the family and patient where they are.
Arly: What has been valuable to your learning and advocacy as an ally?
Dr. Lowery: I have tried to be more involved in the LGBTQIA+ community and I personally tried to educate myself and have meaningful discussions with like minded individuals.
Arly: How do you avoid performative allyship?
Dr. Lowery: I think you avoid performative allyship by actually doing the work. You work on yourself and work on improving the space you occupy.
Arly: Inevitably, mistakes will happen. How do you move past them?
Dr. Lowery: We all make mistakes; when I make a mistake, I try to readily apologize. I also try to be mindful of the situations when/where I made a mistake in order to make me more mindful of times when I may be more apt to make them.
Arly: Why did you feel it was necessary to start an adolescent gender care clinic?
Dr. Lowery: For several years, we had been coordinating care in the background with endocrine and psychology. We decided that it would be better for the patients and families if we were able to coordinate care in one setting.
Arly: What are issues relating to LGBTQ+ patient care that seem to come up time and time again?
Dr. Lowery: Access to gender affirming care [and] finding providers that are affirming can be challenging for families. Additionally, when parents have decided to not affirm their gender diverse children, this can be a challenging situation in which to ally with the teen to help them navigate. Mental health is always in the forefront of providing affirming care, we are always trying to partner with mental health professionals and this can be challenging especially depending on the family’s resources.
Arly: What is one thing you want other healthcare providers to know about providing health care for this population?
Dr. Lowery: Providing gender affirming care is a part of providing general health care. We know that when patients do not feel affirmed they have higher rates of depression, suicidal ideation, and delay in preventative health care. Do not rely on your patients/families to “teach” you. As a provider, it is important to do some self-education. There are some great resources available.
And she is right: there are a great number of resources available to learn how to be a better ally and to learn about LGBTQ+ identities, specific health issues, and experiences. Visit our Resources page for a variety of links or request a training. Feel free to email us at info.grlgbtqhcc@gmail.com if there is a specific resource you are looking for.
Edited for length and clarity.
Dr. Lisa Lowery, MD, MPH, CPE, FAAP, FSAHM (she/her/hers) is an Adolescent Medicine specialist at Helen DeVos Children’s Hospital, where she also serves as the Adolescent Medicine Section Chief and Division Chief of HDVCH Pediatrics Specialties. Dr. Lowery is also Assistant Dean for Diversity and Cultural Initiatives at MSU’s College of Human Medicine, is on the Board of Directors for Grand Rapids LGBTQ+ Healthcare Consortium, the Urban League of West Michigan, and Wedgwood Christian Services. She was one of the Grand Rapids Business Journal’s 50 Most Influential Women in 2022 for her drive, passion, and community impact.